This course is shaped by years of midwives asking for something deeper
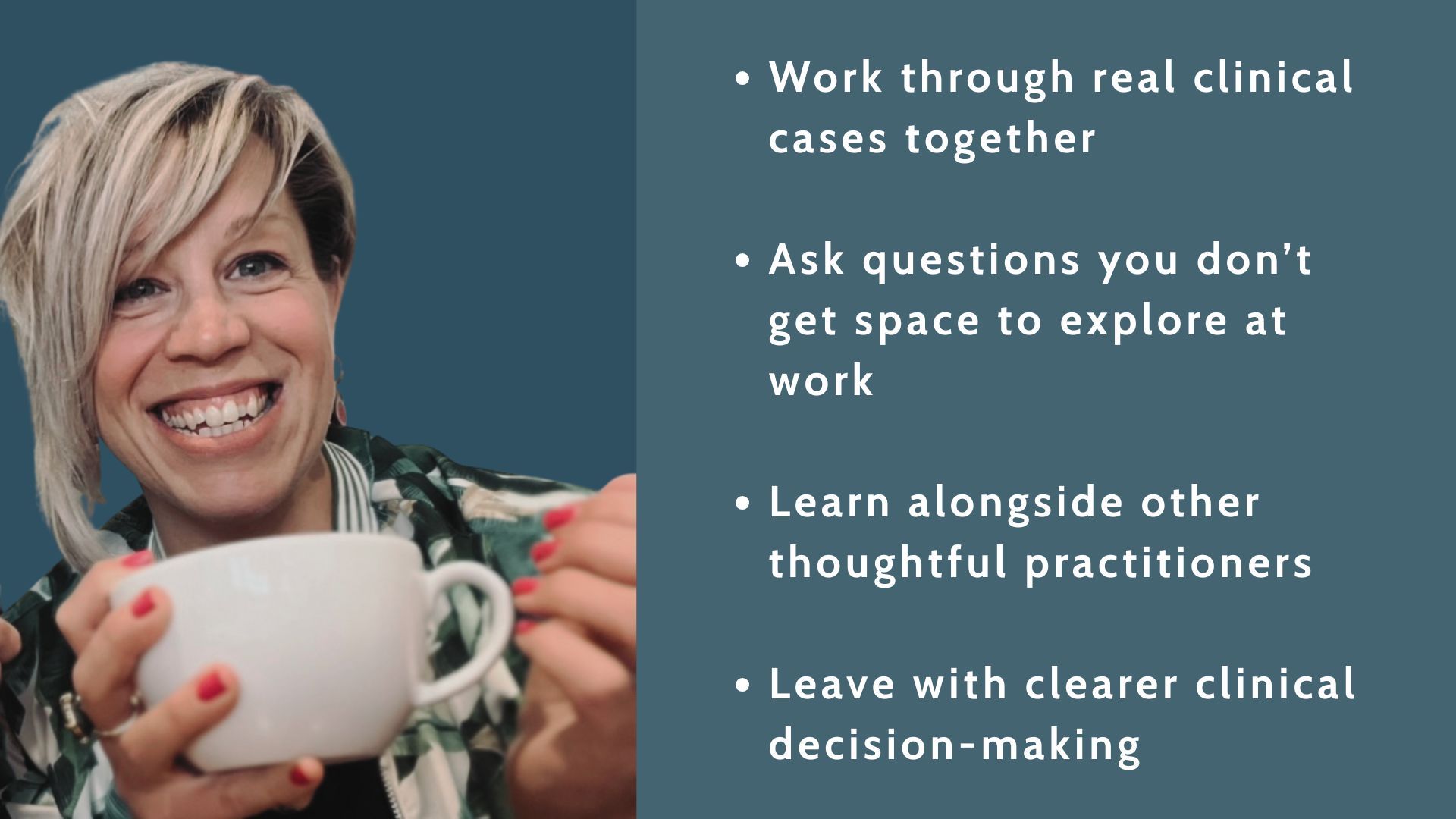
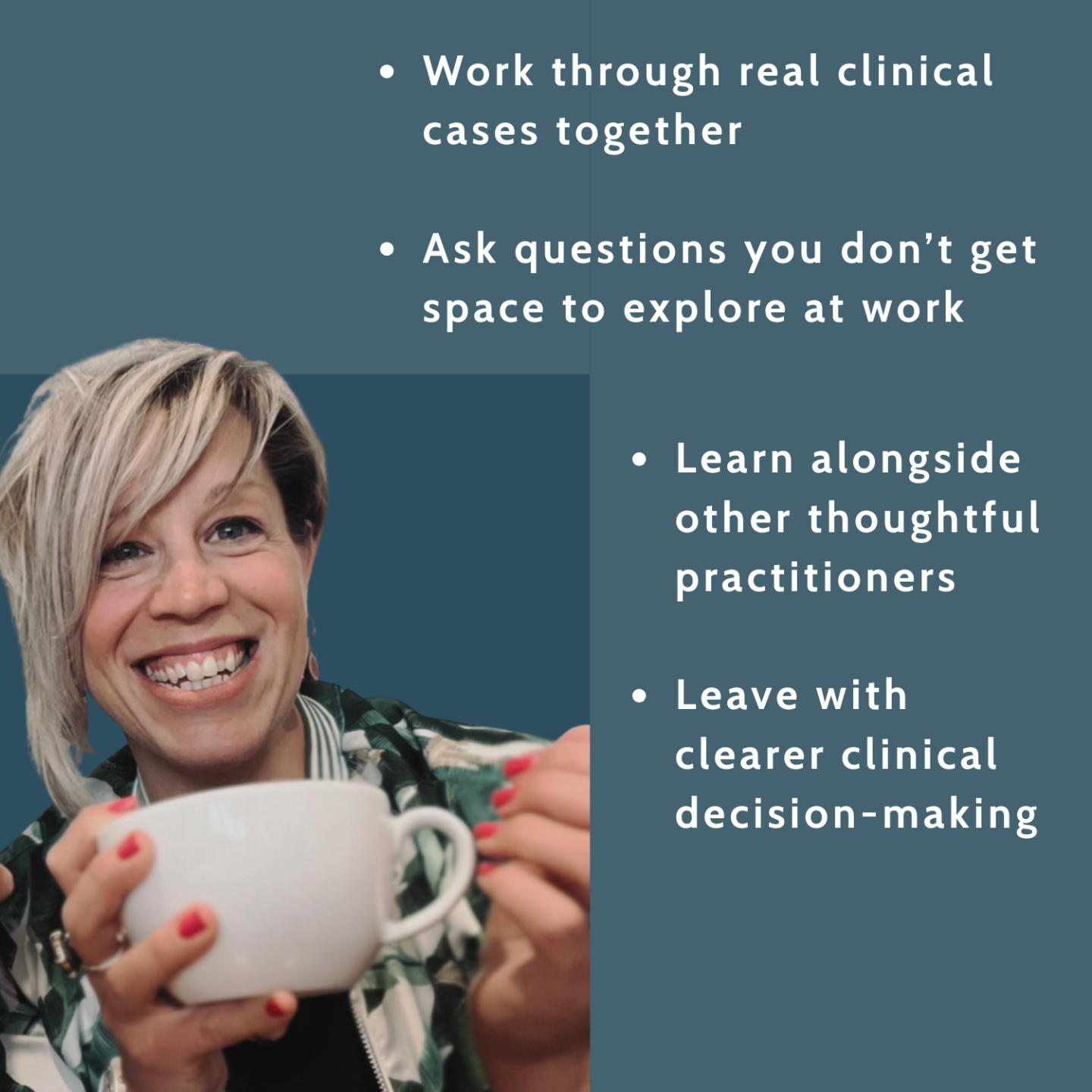
A space to bring real cases.
-
To ask their real questions.
-
To look closely at their own hospital policies.
-
And to develop the ability to see why a particular case has unfolded the way it has — and what would genuinely help next time.
Underneath it all, this course is about building the kind of physiological understanding that makes clinical decision-making calmer, clearer, and more confident — especially in the early days of lactation.
Join the January Cohort ➡Let's Talk live sessions
The breakdown
Weekly 90 min live session themes:
These are not lectures. They are facilitated, case-based discussions designed to help you think more clearly in real clinical situations — using physiology as your guide.
- Week 1 – Starting off right: where breastfeeding support quietly goes wrong
Focus: The earliest hours and days — and why they matter more than most systems acknowledge.
We’ll explore how milk supply is initiated in the immediate post-birth period, and why early decisions — separation, feeding patterns, supplementation, assumptions about “normal” — can quietly shape outcomes long before problems are visible.
You’ll learn how to:
• Recognise early risk factors for delayed or compromised milk production
• Understand which babies and birthing contexts are more vulnerable from the outset
• See how well-intended routines can unintentionally undermine milk supply
• Reframe “normal newborn behaviour” through a physiological lensThis week sets the foundation: once you understand how lactation is meant to begin, the rest starts to make sense.
- Week 2 – Making sense of low milk supply: the building phase and missed windows
Focus: What actually happens when milk supply doesn’t establish as expected — and why.
We’ll work through real clinical cases involving delayed onset of lactation, sleepy or ineffective feeding, early supplementation, and missed stimulation during the critical building phase.
You’ll learn how to:
• Understand milk production as a time-sensitive, responsive system
• Identify when supply is at risk before it is clearly low
• See how early feeding patterns, stimulation, and separation affect long-term capacity
• Explain low milk supply to mums and parents in a way that reduces shame and increases agencyThis is where many practitioners realise they’ve been trying to fix downstream problems without ever being shown how the system was compromised upstream.
- Week 3 – Policy vs physiology: when systems don’t match biology
Focus: How hospital policies interact with lactation physiology — for better or worse.
We’ll examine common term and late-preterm feeding pathways and place them alongside current evidence and biological reality. This is not about blame — it’s about clarity.
You’ll learn how to:
• Read policies through a physiological lens
• Identify where protocols protect milk supply — and where they don’t
• Understand the specific risks faced by late-preterm and vulnerable babies
• Practise questioning and adapting guidelines in ways that are clinically sound and professionally safeThis week helps you move from “I know something isn’t right here” to “I can articulate why — and what would help.”
- Week 4 – From insight to practice: thinking like a detective
Focus: Integration — turning understanding into confident clinical reasoning.
We’ll bring everything together and work through cases where milk supply is already compromised, asking:
What happened? When did it happen? And what can realistically help now?You’ll learn how to:
• Analyse real cases with clearer pattern recognition
• Distinguish between fixable challenges and missed physiological windows
• Support families honestly while preserving confidence and trust
• Use this knowledge to prevent similar issues in future pregnancies
• Teach colleagues or students with clarity rather than overwhelmThis course is not about positioning, attachment, or treating sore nipples — those matter, but they are not the focus here. This cohort is about understanding lactation physiology so clearly that you can see why feeding situations unfold the way they do, and where meaningful intervention is still possible.
YOU DON'T NEED MORE INFORMATION. YOU NEED CLARITY
Next training:
-
Start date: Thursday 22 January
-
End date: Thursday 12 February
-
Live sessions: Thursdays 18:30–20:00 (UK time)
-
Cohort size: Capped at 20
- An Australia-friendly time zone cohort will run later in February / March

-
Your enrollment includes:
-
Access to Breastfeeding & Lactation: The Fundamentals (Modules 1–4) plus case scenarios workbook
-
Four live, case-based teaching sessions
-
Practical, CPD-appropriate learning
-
A small cohort for meaningful discussion
-
This cohort is intentionally small and focused.
You won’t be asked to consume endless material or keep up with daily tasks.
You’ll work through a clear set of foundations, then apply them together in real clinical cases — with space to ask questions, reflect, and think differently.
If you’ve been wanting breastfeeding support to feel clearer, calmer, and more grounded, this is where that shift begins.
Still Got Questions? You're not the only one
Breastfeeding support can feel high-stakes — these are the questions I’m most often asked before people join.

Is this the same as your self-paced course, Breastfeeding & Lactation: The Fundamentals?
Is this the same as the monthly live Q&A sessions?
Is this course about positioning, attachment, or sore nipples?
Who is this course for?
Do I need to attend every live session?
How much time will I need each week?
Will this help me in a busy maternity or hospital setting?
Does this apply only to term babies?
Will this qualify me as a lactation consultant or specialist?
What if I’m not sure this is right for me?
Ready to change how you think in real cases?
Places are limited to keep case discussions meaningful.